- Updated on October 29, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
 All available medical evidence suggests that you can have bronchial asthma only if your breathing is too heavy. You cannot have asthma if you breathe in accordance with medical norms. Therefore, in order to solve problems with asthma and bronchial asthma symptoms, one needs to learn how to breathe correctly.
All available medical evidence suggests that you can have bronchial asthma only if your breathing is too heavy. You cannot have asthma if you breathe in accordance with medical norms. Therefore, in order to solve problems with asthma and bronchial asthma symptoms, one needs to learn how to breathe correctly.
Here is a nice 3D medical asthma animation.
Symptoms and signs of bronchial asthma
Classic bronchial asthma symptoms and signs
 * Bronchoconstriction (narrowing of airways: bronchi and bronchioles) – caused by a CO2 deficiency
* Bronchoconstriction (narrowing of airways: bronchi and bronchioles) – caused by a CO2 deficiency
* Inflammation of airways (caused by cell hypoxia produced by hyperventilation, see CO2: Inflammatory Response)
* Increased sensitivity of the immune system to innocent triggers (dust mites, airborne protein from cats and dogs, pollen, and so forth)
* Excessive production of mucus in airways
Early warning signsIncreased mouth breathing, both during days and night sleep |
Symptoms of mild bronchial asthmaChronic cough, especially at night |
Further development of bronchial asthmaYou can hear yourself wheezing |
Signs of a possible emergency (life-threatening bronchial asthma attack)Severe wheezing while breathing both in and out |
Breathing and causes of asthma
How much do asthmatics breathe?
All available medical research suggests that asthmatics are chronic hyperventilators. Let us review these studies since they explain the key cause of asthma. You can click on the graph to see all references and follow the links to read abstracts of all these 5 studies.
Table. Minute ventilation (asthma)
| Condition | Minute ventilation |
Number of people |
All references or click below for abstracts |
| Normal breathing | 6 L/min | – | Medical textbooks |
| Healthy Subjects | 6-7 L/min | >400 | Results of 14 studies |
| Asthma | 13 (+-2) L/min | 16 | Chalupa et al, 2004 |
| Asthma | 15 L/min | 8 | Johnson et al, 1995 |
| Asthma | 14 (+-6) L/min | 39 | Bowler et al, 1998 |
| Asthma | 13 (+-4) L/min | 17 | Kassabian et al, 1982 |
| Asthma | 12 L/min | 101 | McFadden & Lyons, 1968 |
Note that advanced stages of asthma can lead to lung destruction, ventilation-perfusion mismatch,
and arterial hypercapnia causing further reduction in body oxygen levels.
Chronic hyperventilation causes reduced CO2 levels in alveoli and airways of the lungs. For more details, see causes of asthma.
Can low CO2 levels lead to problems with airways?
 “The mechanism of bronchoconstriction due to hypocapnia in man” (“hypocapnia” means abnormally low CO2 concentrations) was the title of the article published in 1968 by Clinical Science Journal. In this article, Dr. Sterling suggested that CO2 deficiency creates an over-excited state of the cholinergic nerve. Since this nerve is responsible for work of the smooth muscles in bronchi, its excitement leads to constriction of bronchi and smaller air passages (bronchioles). This causes wheezing, coughing, and high heart rate in people with asthma. Mucus production makes these symptoms worse.
“The mechanism of bronchoconstriction due to hypocapnia in man” (“hypocapnia” means abnormally low CO2 concentrations) was the title of the article published in 1968 by Clinical Science Journal. In this article, Dr. Sterling suggested that CO2 deficiency creates an over-excited state of the cholinergic nerve. Since this nerve is responsible for work of the smooth muscles in bronchi, its excitement leads to constriction of bronchi and smaller air passages (bronchioles). This causes wheezing, coughing, and high heart rate in people with asthma. Mucus production makes these symptoms worse.
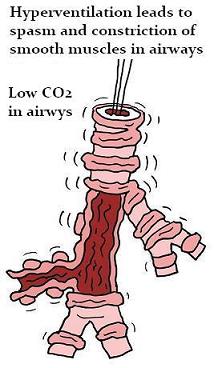 One modern physiology textbook claims, “Agents that tend to dilate human airways include increased PaCO2 (hypoventilation or inspired CO2),” (p. 545; Straub, 1998). This textbook directly asserts that reduced breathing (or hypoventilation) or increased CO2 in the inspired air will dilate airways. Moreover, CO2 is suggested as the most potent natural chemical substance that promotes this “breathing-easy” effect.
One modern physiology textbook claims, “Agents that tend to dilate human airways include increased PaCO2 (hypoventilation or inspired CO2),” (p. 545; Straub, 1998). This textbook directly asserts that reduced breathing (or hypoventilation) or increased CO2 in the inspired air will dilate airways. Moreover, CO2 is suggested as the most potent natural chemical substance that promotes this “breathing-easy” effect.
Soviet MD and Ph.D. KP Buteyko suggested that asthma is caused by alveolar hyperventilation in the 1950’s (his first medical article about this effect was published in 1964). He observed and discovered the central role of breathing too much in the progress and degree of asthma (Buteyko, 1964). He and his medical colleagues also found that asthmatics can get quick alternative drug-free relief from asthma attack symptoms if they practiced shallow or reduced breathing.
Dr. Herxheimer independently suggested that hypocapnia or low CO2 was the cause of bronchial asthma in 1946 (Herxheimer, 1946) and 1952 (Herxheimer, 1952) in his articles “Hyperventilation asthma” and “The late bronchial reaction in induced asthma”.
Allergies and bronchial asthma
How do asthma and asthma attacks develop?
 Low CO2 values in the bronchi cause chronic constriction of airways (that happens in all people). In addition to this direct effect, chronic hyperventilation makes immune reactions abnormal. The immune system becomes too sensitive in relation to intruders from outside (coming with air or food), but weakens the responses to various pathogens, like viruses and bacteria. (That makes sense since hyperventilation is a defensive reaction and a part of the fight-or-flight response. Hyperventilation then should mean a state of increased alertness and emergency for the whole organism, the immune system included.)
Low CO2 values in the bronchi cause chronic constriction of airways (that happens in all people). In addition to this direct effect, chronic hyperventilation makes immune reactions abnormal. The immune system becomes too sensitive in relation to intruders from outside (coming with air or food), but weakens the responses to various pathogens, like viruses and bacteria. (That makes sense since hyperventilation is a defensive reaction and a part of the fight-or-flight response. Hyperventilation then should mean a state of increased alertness and emergency for the whole organism, the immune system included.)
The immune system becomes hypersensitive and seemingly innocent events like breathing cold air or inhaling dust particles can trigger an inflammatory response in asthmatics, excessive production of mucus, a sense of anxiety or panic, more hyperventilation, and further constrictions of airways.
Similar effects take place during physical exercise causing sports induced asthma.
As a result, mucus makes air passages narrower (or even blocks some of them) creating a feeling of suffocation and causing asthma attacks. During an attack, an asthmatic may try to clear the mucus by coughing it out, but that further reduces CO2 concentrations in the lungs and makes air passages narrower. The smart solution to these problems is to do the opposite. How?
This YouTube video (on the right side) provides an overview of problems related to asthma.
Prevention and alternative natural therapy for bronchial asthma
Clinical trials of the Buteyko method for bronchial asthma
 What were the main outcomes of randomized controlled trials of the Buteyko breath therapy in western countries? There were 6 trials altogether. After 3-6 months of daily breathing exercises, asthmatics required:
What were the main outcomes of randomized controlled trials of the Buteyko breath therapy in western countries? There were 6 trials altogether. After 3-6 months of daily breathing exercises, asthmatics required:
– 3-9 times less reliever medication
– about 2 times less steroidal drugs
– significantly improved quality of life
– significantly improved score for asthma symptoms (less cough, wheezing, chest tightness, dyspnea, and other symptoms of asthma).
All these astonishing results in spite of the fact that if we compare pulmonary parameters of the patients in the experimental groups at the end of the trials, they only partially normalized their breathing achieving about 25-30 seconds CP (the body-oxygen test described below).
You can read all abstracts and detailed results of these and other trials: Clinical Trials of the Buteyko Method.
However, there were no changes in lung function results. Why? According to Dr. Buteyko’s theory of breathing, normalization must cure asthma. Did asthmatics change their breathing during these randomized controlled trials? During the most impressive study in Australia (Bowler et al, 1998),
in 3 months, consumption of reliever medication was reduced by 96% (or 25 times less) and inhaled steroidal drugs or preventers by about 50%. Respiratory minute volume at rest decreased from initial 14 L/min to 9.6 L/min after 3 months, but the medical norm for breathing is only 6 L/min, while Dr. Buteyko’s standard is 4 L/min at rest for a 70-kg man. Hence, during their best shot, the participated asthmatics got only about a half way towards the standard. Thus, there were a very few asthmatics, if any, who naturally normalized their breath during these trials.
One of the assumptions of the medical doctors, who participated in these asthma trials, was that a Buteyko therapist taught the alternative Buteyko technique, while a controlled group of asthmatics learned the therapy. Indeed, in titles and abstracts of these randomized controlled trials, we can read “trial of the Buteyko method”. How could they study the Buteyko breathing method, if no one learned it?
 If we consider these trials from a practical viewpoint, the patients were mainly limited to practicing breathing exercises (e.g., 1 hour per day). However, breathing retraining requires constant regulation of breathing due to the negative effects of lifestyle risk factors. As we already learned it in the past, asthmatics are most likely to die and experience acute episodes and attacks during early morning hours due to the Morning Hyperventilation Effect. What is the point to treat asthma, if most asthmatics sleep on their backs and breathe through the mouth during sleep (hence, dry mouth in the morning)?
If we consider these trials from a practical viewpoint, the patients were mainly limited to practicing breathing exercises (e.g., 1 hour per day). However, breathing retraining requires constant regulation of breathing due to the negative effects of lifestyle risk factors. As we already learned it in the past, asthmatics are most likely to die and experience acute episodes and attacks during early morning hours due to the Morning Hyperventilation Effect. What is the point to treat asthma, if most asthmatics sleep on their backs and breathe through the mouth during sleep (hence, dry mouth in the morning)?
They will surely produce more irritation of airways, inflammation, and mucus during mouth breathing. How could they heal their airways if their irritate them every morning? The typical daily CPs (body-oxygen test results – see below) at the end of trials, judging by other respiratory parameters, were about 20-30 s. Morning CPs were around 15-22 s. This allows, according to Buteyko Table of Health Zones, reduction in most medication for asthma, but has never been enough to heal airways and normalize lung function results.
Hence, it is not a smart way to teach breathing retraining therapy without:
– nose breathing all the time; mouth taping at night
– avoidance of sleeping on one’s back (it causes higher heart rate and even chest pain)
– correct coughing techniques and wheezing (ordinary coughing increases production of mucus)
– sufficient physical activity (at least 2 hours every day with nasal breathing only)
– and numerous other lifestyle-related details so that one’s basal breathing pattern is gradually restored back to the medical international standard.
There are 3 levels to defeat asthma. The concise details (what is required to achieve) for these 3 levels are hidden as your bonus content below here.
Level 1. Learn how to stop asthma attacks with reduced breathing exercise.
Level 2. Get 20-25 s for the morning CP. This will reduce your medication intake to nothing or nearly nothing.
Level 3. Get over 50 s for the morning CP. This will eliminate inflammation in less than 3 weeks.
Therefore, when a breathing student normalizes his or her automatic breathing patterns, he or she will have a complete clinical remission (cure) from asthma.
[/sociallocker]
Coughing and acute asthma web pages:
– Stop Acute Asthma Exacerbation in 2-3 min (Breathwork)
– Stop Coughing At Night – A breathing exercise to reduce the duration and severity of coughing at night. This exercise helps to fall asleep faster
– Best Cough Treatment Therapy – The ultimate solution to chronic problems with wet or whooping cough, chesty of a dry cough, coughing at night, and coughing in children.
Further resources:
– Acute Asthma Exacerbations Clinical Trial – Application of the Frolov breathing device in a hospital setting: probably the most successful medical trial in the history of asthma trials
– Clinical effects of the Buteyko breathing technique on asthma and other respiratory disorders – Whatever the breathing technique applied, the final results for over 95% of breathing students depend only on their morning CP achieved.
Medical references
Buteyko KP, An Instruction for VBN Therapy for Bronchial Asthma, Angina Pectoris, High Blood Pressure and Obliterating Endarteritis: Preprint. – Novosibirsk, 1964.
Herxheimer H, Hyperventilation asthma, Lancet 1946, 6385: p. 83-87.
Herxheimer H, The late bronchial reaction in induced asthma, Int Arch Allergy Appl Immunol 1952; 3: p. 323-328.
Straub NC, Section V, The Respiratory System, in Physiology, eds. RM Berne & MN Levy, 4-th edition, Mosby, St. Louis, 1998.


