- Updated on October 29, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
In this YouTube video, Dr. Artour shares great experience of Buteyko breathing teachers to treat CFS-ME-Fibromyalgia naturally using the Buteyko technique and breathing retraining.
If we consider mainstream medical definitions of chronic fatigue syndrome, we can easily notice that the listed symptoms include heavy breathing and chest pain. Among other possible symptoms are muscle pain, shortness of breath, night sweats, chronic headaches, muscle fatigue, cramps and spasms, cold hands and feet, extreme fatigue and weakness. These are all classical symptoms and signs of chronic hyperventilation, which causes low body-oxygen levels.
What causes chronic fatigue?
 As we explained before, heavy breathing (or breathing more than the medical norm) reduces body-oxygen content due to 3 independent mechanisms:
As we explained before, heavy breathing (or breathing more than the medical norm) reduces body-oxygen content due to 3 independent mechanisms:
1) since CFS (or Chronic Fatigue Syndrome) patients are chest breathers, chest breathing reduces oxygenation of the arterial blood due to insufficient ventilation and oxygenation of the lower parts of the lungs
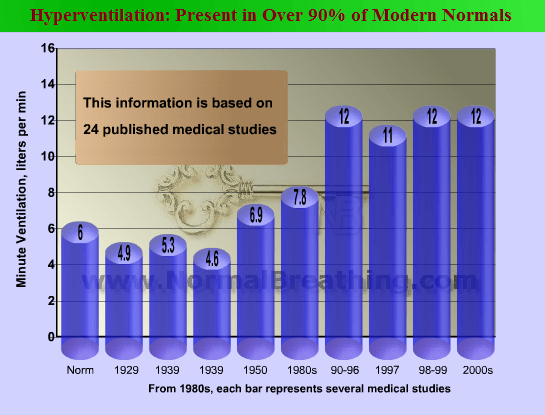
2) CO2 deficiency, due to breathing too much, causes constriction of arteries and arterioles, reducing blood supply to tissues since CO2 is a vasodilator (see links below).
3) Less oxygen is released by hemoglobin cells in tissues due to the suppressed Bohr effect (caused by CO2 deficiency as well).
The link between chronic fatigue syndrome and ineffective breathing was suggested by many doctors. Some of the quotes (Rosen et al, 1990; Paulley, 1990) are provided in the references below. These doctors directly claim that the label “chronic fatigue” means hyperventilation. Measured end-tidal CO2 values are below the norm in CFS patients (Razumovsky et al, 2003; Cook et al, 2006; Natelson et al, 2007) and end-tidal CO2 is even less during acute episodes (Bogaerts et al, 2007).
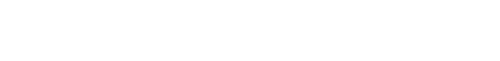
 Note. In some studies, medical doctors suggested that low end-tidal CO2, e.g., less than 30 mm Hg (!), is the criteria of hyperventilation (Naschitzet al, 2006, Saisch et al, 1994). The typical borderline is 35 mm Hg. Furthermore, it is a known fact that hyperventilation or overbreathing can be present while having perfectly normal end-tidal CO2 parameters at rest (e.g., due to predominantly chest breathing and/or ventilation/perfusion mismatch) and that hyperventilation means to have abnormally high pulmonary ventilation (or minute ventilation). Thus, hyperventilation is alveolar hyperventilation only.
Note. In some studies, medical doctors suggested that low end-tidal CO2, e.g., less than 30 mm Hg (!), is the criteria of hyperventilation (Naschitzet al, 2006, Saisch et al, 1994). The typical borderline is 35 mm Hg. Furthermore, it is a known fact that hyperventilation or overbreathing can be present while having perfectly normal end-tidal CO2 parameters at rest (e.g., due to predominantly chest breathing and/or ventilation/perfusion mismatch) and that hyperventilation means to have abnormally high pulmonary ventilation (or minute ventilation). Thus, hyperventilation is alveolar hyperventilation only.  (Are functioning alveoli ventilated in accordance with metabolic needs and corresponding to the norm, which is 6 L/min for minute ventilation at rest for a 70-kg man?). There are no any other types of hyperventilation.
(Are functioning alveoli ventilated in accordance with metabolic needs and corresponding to the norm, which is 6 L/min for minute ventilation at rest for a 70-kg man?). There are no any other types of hyperventilation.
Hyperventilation should cause symptoms of chronic fatigue syndrome
When muscle cells and other metabolically active tissues of the human body do not get enough oxygen supply, more mitochondria switch from an aerobic to an anaerobic energy-production mechanism. This causes elevated lactic acid content in tissues and blood, together with the main symptoms of lactic acid: weakness, fatigue, and pain in muscles and the chest (heart muscle tissue also gets less oxygen and suffers from tissue hypoxia). Apart from lowered oxygenation and blood supply to the brain, heavy breathing makes nerve cells overexcited and irritable, causing headaches and anxiety problems.
 Chronic overbreathing creates cell hypoxia, elevated lactic acid, constant production of free radicals in cells, free radicals damage, possible inflammation in various areas of the body, leading to decreased vagal power (Sisto et al, 1995), blocked nose and chronic sinusitis, digestive problems, face acne, liver inflammation (with abnormal liver test results), and many other pathological effects. Inflammatory processes and the mental state of chronic stress (fight-or-flight response) exhaust cortisol reserves (cortisol is a steroid hormone or glucocorticoid produced by the adrenal gland). This explains how Adrenal Fatigue Syndrome and chronic insufficiency in cortisol reserves develop.
Chronic overbreathing creates cell hypoxia, elevated lactic acid, constant production of free radicals in cells, free radicals damage, possible inflammation in various areas of the body, leading to decreased vagal power (Sisto et al, 1995), blocked nose and chronic sinusitis, digestive problems, face acne, liver inflammation (with abnormal liver test results), and many other pathological effects. Inflammatory processes and the mental state of chronic stress (fight-or-flight response) exhaust cortisol reserves (cortisol is a steroid hormone or glucocorticoid produced by the adrenal gland). This explains how Adrenal Fatigue Syndrome and chronic insufficiency in cortisol reserves develop.
Particularly, for most patients, symptoms of chronic fatigue are worst during early morning hours (Togo et al, 2008; Guilleminault et al, 2008). 
Therefore, the cause of chronic fatigue syndrome is overbreathing or hyperventilation. There were many doctors who suggested this link, but Dr. Buteyko and his medical colleagues went further, developing the medical program for the natural treatment of chronic fatigue syndrome using the Buteyko breathing method of breathing retraining.
When the cause is removed (due to breathing normalization or breathing retraining), all symptoms of fatigue, including chest pain, shortness of breath, night sweats, muscle pain and fatigue, chronic headaches, and weakness, naturally disappear.
Chronic fatigue syndrome and body-oxygen levels
The degree of chronic fatigue syndrome in an individual can be found using a stress-free body-oxygen test, which measures one’s body oxygenation in seconds.
| Body-oxygen level | Symptoms (Chronic Fatigue Syndrome) |
| 1-10 s | Extreme fatigue syndrome; severe chest tightness; night sweats; severe dyspnea; severe muscle pain; severe chronic headaches |
| 11-20 s | Moderate fatigue; chest pain; weakness; mild chest pain; shortness of breath; muscle pain |
| 20-40 s | Moderate level of energy; possible desire to slouch; light muscle pain; night sweats and headaches are very rare |
| Over 40 s | Craving and joy of physical exercise; the attention is focused on the outer world instead of bodily pains and aches |
 As an additional test, measure your heart rate since the pulse of chronic fatigue disorder patients is above the norm. The normal pulse rate is about 60-70 beats per minute. Patients with a moderate degree of chronic fatigue syndrome often have more than 80 beats per minute at rest, while sitting. When the body oxygenation is below 10 s, the heart rate is often more than 90 beats per minute.
As an additional test, measure your heart rate since the pulse of chronic fatigue disorder patients is above the norm. The normal pulse rate is about 60-70 beats per minute. Patients with a moderate degree of chronic fatigue syndrome often have more than 80 beats per minute at rest, while sitting. When the body oxygenation is below 10 s, the heart rate is often more than 90 beats per minute.
When a person suffers from Adrenal Fatigue Syndrome with an insufficient blood cortisol level, the adrenal gland does not recover if his or her body-oxygen content is below 20 s. Once a person has more than 20 s, any additional supplementation in cortisol is not required. Note that some patients with chronic and extreme fatigue, if they decide to improve their breathing, require cortisol supplementation so that they can progress and get higher body oxygenation numbers.
Natural Treatment for Chronic Fatigue Syndrome
 All symptoms of chronic fatigue syndrome including muscle pain, breathlessness, night sweats, headaches, and weakness will disappear if one normalizes his or her automatic or unconscious breathing pattern. Breathing retraining, so that one breathe differently 24/7, requires lifestyle changes for better body oxygenation and breathing exercises that can make breathing lighter and slower. It is a serious project, which is explained in detail in the Learn here Section. Note that many western MDs also consider breathing retraining as the way to deal with the chronic fatigue disorder (Nijs et al, 2007; Vasiliauskas et al, 2008).
All symptoms of chronic fatigue syndrome including muscle pain, breathlessness, night sweats, headaches, and weakness will disappear if one normalizes his or her automatic or unconscious breathing pattern. Breathing retraining, so that one breathe differently 24/7, requires lifestyle changes for better body oxygenation and breathing exercises that can make breathing lighter and slower. It is a serious project, which is explained in detail in the Learn here Section. Note that many western MDs also consider breathing retraining as the way to deal with the chronic fatigue disorder (Nijs et al, 2007; Vasiliauskas et al, 2008).
Amazing medical references: 15 clinical studies claim that chronic fatigue means hyperventilation
There are 15 astonishing medical studies that link chronic fatigue with overbreathing. You can see references for these studies further down this page.
Medical References
Rosen SD, King JC, Wilkinson JB, Nixon PG, Is chronic fatigue syndrome synonymous with effort syndrome? Journal of the Royal Society of Medicine, 1990 Dec; 83(12): 761-764.
Paulley JW, Hyperventilation, Recent Progress in Medicine 1990 Sep; 81(9): 594-600.
Bogaerts K, Hubin M, Van Diest I, De Peuter S, Van Houdenhove B, Van Wambeke P, Crombez G, Van den Bergh O., Hyperventilation in patients with chronic fatigue syndrome: the role of coping strategies, Behav Res Ther. 2007 Nov; 45(11): p. 2679-2690. Epub 2007 Jul 20.
Vasiliauskas D1, Kavoliūniene A, Jasiukeviciene L, Grizas V, Statkeviciene A, Leimoniene L, Tumyniene V, Kubilius R., [Impact of a long-term complex rehabilitation on chronic fatigue and cardiorespiratory parameters in patients with chronic heart failure], Medicina (Kaunas). 2008;44(12):911-21.
Hypocapnia or low end-tidal CO2 in chronic fatigue syndrome
Bazelmans E, Bleijenberg G, Vercoulen JH, van der Meer JW, Folgering H., The chronic fatigue syndrome and hyperventilation, J Psychosom Res. 1997 Oct;43(4):371-7
Cook DB, Nagelkirk PR, Poluri A, Mores J, Natelson BH., The influence of aerobic fitness and fibromyalgia on cardiorespiratory and perceptual responses to exercise in patients with chronic fatigue syndrome, Arthritis Rheum. 2006 Oct; 54(10): p. 3351-62.
Guilleminault C, Poyares D, Rosa A, Kirisoglu C, Almeida T, Lopes MC, Chronic fatigue, unrefreshing sleep and nocturnal polysomnography, Sleep Med. 2006 Sep;7(6):513-20. Epub 2006 Aug 24
Lee S., Estranged bodies, simulated harmony, and misplaced cultures: neurasthenia in contemporary Chinese society, Psychosom Med. 1998 Jul-Aug; 60(4): p. 448-457.
Naschitz JE, Mussafia-Priselac R, Kovalev Y, Zaigraykin N, Slobodin G, Elias N, Rosner I., Patterns of hypocapnia on tilt in patients with fibromyalgia, chronic fatigue syndrome, nonspecific dizziness, and neurally mediated syncope, Am J Med Sci. 2006 Jun;331(6): p. 295-303.
Natelson BH, Intriligator R, Cherniack NS, Chandler HK, Stewart JM., Hypocapnia is a biological marker for orthostatic intolerance in some patients with chronic fatigue syndrome, Dyn Med. 2007 Jan 30;6:2.
Nijs J, Adriaens J, Schuermans D, Buyl R, Vincken W., Breathing retraining in patients with chronic fatigue syndrome: a pilot study. Physiother Theory Pract. 2008 Mar-Apr;24(2):83-94.
Razumovsky AY, DeBusk K, Calkins H, Snader S, Lucas KE, Vyas P, Hanley DF, Rowe PC., Cerebral and systemic hemodynamics changes during upright tilt in chronic fatigue syndrome, J Neuroimaging. 2003 Jan; 13(1): p. 57-67.
Saisch SG, Deale A, Gardner WN, Wessely S., Hyperventilation and chronic fatigue syndrome, Q J Med. 1994 Jan;87(1):63-7.
Sisto SA, Tapp W, Drastal S, Bergen M, DeMasi I, Cordero D, Natelson B., Vagal tone is reduced during paced breathing in patients with the chronic fatigue syndrome, Clin Auton Res. 1995 Jun; 5(3): p. 139-143.
Togo F, Natelson BH, Cherniack NS, FitzGibbons J, Garcon C, Rapoport DM., Sleep structure and sleepiness in chronic fatigue syndrome with or without coexisting fibromyalgia, Arthritis Res Ther. 2008;10(3):R56. Epub 2008 May 13.