- Updated on September 11, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
Effects of Exercise on the Respiratory System: Short- and Long-Term CO2 changes
 Effects of physical activity and sports on the respiratory system mainly depend on changes in alveolar CO2 levels. Here, after analyzing the basics of oxygen transport (changes in CO2 and O2 concentrations in the blood and cells), we are going to provide clear and simple answers to the following questions:
Effects of physical activity and sports on the respiratory system mainly depend on changes in alveolar CO2 levels. Here, after analyzing the basics of oxygen transport (changes in CO2 and O2 concentrations in the blood and cells), we are going to provide clear and simple answers to the following questions:
– What are the exact criteria that determine the long-term positive effects of exercise on overall health and well-being?
– Are these criteria different in healthy and sick people?
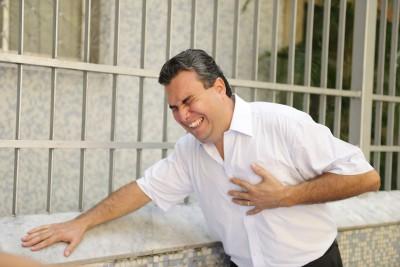
– If exercise is healthy, why do thousands of sick people die every year from coronary-artery spasms, anginas, infarcts, strokes, exercise-induced asthma attacks and many other acute exacerbations of diseases during or following physical exercise?
– Is graded exercise therapy useful for all patients?
– What is going on with the respiratory system of these people during exercise?
– What are the short-term and long-term effects of exercise on the respiratory system?
Table. MV (Minute Ventilation) and Rf (Respiratory Frequency) at rest
| Condition | MV, L/min | Rf, breaths/min | Oxygen extraction, % |
Breath pattern | References (click below for details) |
| Diseases* | 12-18 | >18 | <12 % | Overbreathing | Over 40 studies |
| Healthy | 6-7 | 10-12 | 25 % | Normal | Results of 14 studies |
| Norm | 6 | 12 | 25 % | Normal | Medical textbooks |
| Super-health | 2 | 3 | >60 % | Ideal | Observations/yoga |
*Chronic diseases include heart disease, diabetes, asthma, COPD, cystic fibrosis, cancer, and many others. Study Hyperventilation Syndrome for references and numbers.
As it is easy to observe, heavy breathing at rest results in relatively heavy breathing during exercise and that makes moderate or intensive exercise in the sick very difficult or impossible.
Table. Minute ventilation during moderate exercise (15-fold metabolism)
| Condition | Minute ventilation |
Short-term respiratory effects | Blood lactate | Duration of performance |
| Chronic diseases | About 150 L/min | Maximum mouth ventilation | Very high | A few minutes |
| Normal breathing | 90 L/min | Heavy nose breathing | Elevated | 1-2 hours |
| Super health states | 30 L/min | Easy nose breathing | Nearly normal | Many hours |
 If you attend a typical mass running event or open marathon, you will notice numerous ambulances with paramedics, who are ready to provide rescue help and oxygen, regardless of the details of the chronic disease (heart disease, stroke, seizures, exercise-induced asthma, and so forth). Whatever the condition, low brain and heart oxygen levels are most likely physiological causes of possible deaths. Hence, the main questions then are: What are the factors that define the effects of exercise on the respiratory system? What is going on with blood gases or O2 and CO2 in the blood and body cells? The answers depend on the pre-existing respiratory parameters and levels of blood gases before and after exercise.
If you attend a typical mass running event or open marathon, you will notice numerous ambulances with paramedics, who are ready to provide rescue help and oxygen, regardless of the details of the chronic disease (heart disease, stroke, seizures, exercise-induced asthma, and so forth). Whatever the condition, low brain and heart oxygen levels are most likely physiological causes of possible deaths. Hence, the main questions then are: What are the factors that define the effects of exercise on the respiratory system? What is going on with blood gases or O2 and CO2 in the blood and body cells? The answers depend on the pre-existing respiratory parameters and levels of blood gases before and after exercise.
Effects of Exercise and the respiratory system in healthy people
 Considerthe short-term effects of exercise in healthy people. Textbooks on exercise physiology suggest that, in fit and healthy people, arterial CO2 levels rise slightly with light, moderate, medium and sub-maximum exercise intensity levels regardless of the route of breathing during exercise (mouth or nasal or combined). Since CO2 is the powerful vasodilation agent, expanded arteries and arterioles improve blood and O2 delivery to all vital organs of the human body, including the heart and brain. Vasodilation ensures aerobic respiration in body cells making it possible for healthy people to enjoy all the benefits of aerobic exercise without any major problems related to tissue hypoxia causing excessive blood lactate, muscle spasms, injuries, low recovery rates, overexcitement, stress, poor sleep later, etc.
Considerthe short-term effects of exercise in healthy people. Textbooks on exercise physiology suggest that, in fit and healthy people, arterial CO2 levels rise slightly with light, moderate, medium and sub-maximum exercise intensity levels regardless of the route of breathing during exercise (mouth or nasal or combined). Since CO2 is the powerful vasodilation agent, expanded arteries and arterioles improve blood and O2 delivery to all vital organs of the human body, including the heart and brain. Vasodilation ensures aerobic respiration in body cells making it possible for healthy people to enjoy all the benefits of aerobic exercise without any major problems related to tissue hypoxia causing excessive blood lactate, muscle spasms, injuries, low recovery rates, overexcitement, stress, poor sleep later, etc.
Hence, healthy people experience immediate positive effects of exercise on the respiratory system and blood gases. What happens after exercise (long-term effects of exercise on the respiratory system)? Since breathing is controlled by CO2, the usual exercise effects for fit and healthy people are simple: breathing after exercise becomes lighter and slower due to an adaptation of the respiratory system and the breathing center to higher CO2 levels. As a result, the body-oxygen content increases for many hours after the exercise. This especially relates to the next-morning body oxygenation, and this is the main criterion of exercise efficiency if someone decides to measure the exact long-term effects of exercise on the respiratory system.
However, when very healthy and healthy people do exercise with strictly nasal breathing, their blood gases during exercise are different in comparison with mouth breathing. Arterial CO2 gets even higher, and arterial oxygen saturation becomes slightly less in a dose-dependent manner. Nasal breathing (in and out) slightly worsens the immediate performance and results but is incomparably better in the long run. Why? Intermittent hypoxic hypercapnic training, as in case of nose breathing (in and out), is an excellent way to improve VO2 max, body-oxygen content and achieve adaptation of the breathing center to higher CO2.
VO2max (definition)= the maximal oxygen uptake or the maximum volume of oxygen that can be utilized by the human body in one minute during maximal exercise. It is measured as milliliters of oxygen used in one minute per kilogram of body weight (ml/kg/min). VO2max is usually ranged from 20-40 ml/kg/min (in unfit and ordinary subjects) and up to 80-90 ml/mg/min (in elite endurance athletes). Physiologically, it is the most significant parameter that predicts long-term endurance and performance in athletes.
One can try both these approaches (reduced nasal breathing on some days and heavy mouth breathing in others) and compare the effects of both types of exercise on your well-being. It is, for example, easy to discover that physical exercise with strictly nose breathing significantly reduces pulse for the same intensity level for any particular individual in comparison with mouth or combined breathing. Hence, the positive effects of physical exercise with nasal breathing only are immediate. They can be easily measured with sports watches and other devices that can record heart rate during exercise.
Exercise and the respiratory system in sick people
 As analyzed before (see links below for over 40 medical studies that measured breathing in groups of sick people), sick people have heavy and deep breathing at rest before exercise. Hence, there have abnormal blood gases prior to exercise. Usually, they suffer from arterial hypocapnia (low CO2 due to overbreathing) and (likely) mild arterial hypoxia if they are chest breathers. (Chest breathing, as we discussed, reduces the oxygen level in the arterial blood.)
As analyzed before (see links below for over 40 medical studies that measured breathing in groups of sick people), sick people have heavy and deep breathing at rest before exercise. Hence, there have abnormal blood gases prior to exercise. Usually, they suffer from arterial hypocapnia (low CO2 due to overbreathing) and (likely) mild arterial hypoxia if they are chest breathers. (Chest breathing, as we discussed, reduces the oxygen level in the arterial blood.)
If they have problems with their lungs or ventilation-perfusion mismatch (as in a small group of patients with severe asthma, bronchitis, or emphysema), their arterial CO2 is too high (up to 50-60 mm Hg), but blood oxygenation is low already at rest, causing dyspnea (shortness of breath sensation) even during low-intensity exercise.
 Overbreathing at rest reduces their body-oxygen levels. As a result, many people with diabetes, cancer, heart disease, chronic fatigue and many other conditions have elevated blood lactate level at rest, indicating the presence of cell hypoxia and anaerobic cellular respiration. Mild exercise generates even more lactic acid due to initial oxygen deficiency. (This is the common reason why the sick people do not like exercise.) As a result, since the lactic acid level is also controlled by the respiratory system, the body starts to remove bicarbonates (CO2) from the blood by increased ventilation (metabolic acidosis). To maintain blood pH in the normal range, the breathing center intensifies minute ventilation to remove some CO2 from the body. The breathing becomes disproportionally heavier (the main short-term effect of exercise in the sick). This is possible to observe in many sick people during exercise: heavy panting, usually through the wide open mouth.
Overbreathing at rest reduces their body-oxygen levels. As a result, many people with diabetes, cancer, heart disease, chronic fatigue and many other conditions have elevated blood lactate level at rest, indicating the presence of cell hypoxia and anaerobic cellular respiration. Mild exercise generates even more lactic acid due to initial oxygen deficiency. (This is the common reason why the sick people do not like exercise.) As a result, since the lactic acid level is also controlled by the respiratory system, the body starts to remove bicarbonates (CO2) from the blood by increased ventilation (metabolic acidosis). To maintain blood pH in the normal range, the breathing center intensifies minute ventilation to remove some CO2 from the body. The breathing becomes disproportionally heavier (the main short-term effect of exercise in the sick). This is possible to observe in many sick people during exercise: heavy panting, usually through the wide open mouth.

Mouth breathing, as we’ve previously discussed, further reduces the arterial and cellular CO2, creating brain hypoxia and increasing heart rate. Nasal breathing, on the other hand, prevents CO2 and nasal NO (nitric oxide) losses and improves brain and heart-oxygen content provided that the intensity of exercise matches oxygen delivery.
The overbreathing caused by mouth breathing during exercise can continue for many hours after exercise if it is too intensive or anaerobic. Exercise with low intensities are better tolerated, but mouth breathing still negates any improvements in heart and body oxygen level canceling positive long-term effects of exercise on the respiratory system. It is normal then that severely-sick individuals can easily die due to moderate or intensive exercise combined with other hyperventilation-inducing lifestyle factors, including stress, overheating, overeating before the exercise, drop in blood glucose level, chest breathing, etc. It is not a surprise then that graded exercise therapy has conflicting results so far.
There are many coaches and fitness instructors these days who teach their athletes, students, and pupils to breathe in through the nose and out through the mouth in order to improve long-term effects of exercise on the respiratory system. This breathing technique for physical exercise is half-better than mouth breathing due to improved absorption of nitric oxide and some increase in arterial CO2.
Conclusion. The effects of exercise on the respiratory system and body-oxygen content in the sick are generally negative due to mouth breathing. There are, however, somepositive effects of exercise due to perspiration, shaking of the body, stimulation of the respiratory muscles and lungs, production of endorphins, and others.

Which exercise programs have the best short-term and long-term effects on the respiratory system and body oxygen content?
Clinical experience of a large group of Soviet and Russian MDs suggests that nasal breathing during exercise is the key factor that maximizes positive short- and long-term effects of exercise on the respiratory system, and prevents any acute episodes, including coronary spasms, angina pains, infarcts, strokes, sport-induced asthma attacks, and seizures. Furthermore, nasal breathing ensures absorption of nitric oxide generated in the sinuses and inhaled into the lungs during nose breathing.
Consider how nasal breathing provided good health for people in the past. Physical exercise was the main factor that made the breathing and body-oxygen content of our predecessors much better. They were exercising up to 8-12 hours per day (including walking, gardening, and all type of activities where the whole body is involved in movement). Mouth breathing, as you can easily see in old photos and movies, was a socially unacceptable habit. Some evidence suggests that even competing athletes were breathing strictly through the nose (in and out) during training sessions and sports contests.
 With the advance of the industrial revolution during the last 100 years, the amount of average exercise for people declined down to 10-60 min per day (this includes walking). Furthermore, mouth breathing during exercise leads to heart attacks, strokes, exercise-induced asthma attacks, and other exacerbations. As a result, physical exercise, instead of being a health benefit, became a serious hazard since we lost the habit of nose breathing. However, all the adverse long-term and short-term effects of exercise on the respiratory system can be virtually eliminated via the use of strictly nasal breathing (in and out).
With the advance of the industrial revolution during the last 100 years, the amount of average exercise for people declined down to 10-60 min per day (this includes walking). Furthermore, mouth breathing during exercise leads to heart attacks, strokes, exercise-induced asthma attacks, and other exacerbations. As a result, physical exercise, instead of being a health benefit, became a serious hazard since we lost the habit of nose breathing. However, all the adverse long-term and short-term effects of exercise on the respiratory system can be virtually eliminated via the use of strictly nasal breathing (in and out).
Hence, the oldest or traditional exercise programs (physical activity with nasal breathing only) have the best effects on the respiratory system and body-oxygen levels and general health of humans due to the high CO2 production rate, arterial CO2 increases, an adaptation of the breathing center to higher CO2 with slower and lighter automatic breathing for many hours later.
“Physical work, sport, and exertion increase CO2 production. Its level increases in the blood, while oxygen decreases. The higher the intensity, the stronger the excitement of the breathing center and the deeper the breathing, but it is only deeper formally. Breathing becomes not deeper, but shallower: it is less in relation to metabolism. This is the reasoning behind the usefulness of exercise and sport! During prolonged intensive exercise the receptors, which control breathing, adapt to increased CO2. If the person regularly works and toils, then he practically follows our method: he is decreasing his breathing using exercise”. Dr. Buteyko lecture in the Moscow State University on 9 December 1969
Physical exercise, according to Dr. Buteyko, is the main factor that defines the long-term success of the student during breathing retraining due to the positive effects of exercise on the respiratory system. Since a lack of physical exercise is the main cause of hyperventilation in modern man, it is normal that daily duration of physical activity has a correlation with personal-morning body-oxygen content (the CP – control pause). Indeed, Buteyko and his colleagues found that when their students achieved high CPs (e.g., up to 60 s) and stopped doing breathing exercises, the stability of their CPs was dependent on the amount of their daily physical exercise.
If you want to know how much exercise is possible and easy to have for super health states, and if you want to know 2 key factors, apart from nose breathing, that makes exercise effective, you can find these details as your bonus content below here.
1. For people with super-health states (about 2-3 min for the body-oxygen test), with 3-4 hours of daily intensive exercise (and that is pleasant for them), it is easy to maintain their ideal-body-oxygen levels.
2. It is particularly beneficial to Effects of exercise when a session is accompanied by perspiration (sweating) and prolonged shaking (mechanical vibrations of the body), as, for example, during jogging.
[/sociallocker]
Sport and fitness articles:
– Simple breathing exercise for higher VO2max
– Increase VO2max by breathing differently at rest
– Exercise is joy if the body is oxygenated at rest
– When exercise is 100% safe for chronic diseases
– Why modern man gets little, if any, benefits from exercise
– Which exercise parameters increase body oxygenation
Medical references
Clark AL, Volterrani M, Swan JW, Coats AJS, The increased ventilatory response to exercise in chronic heart failure: relation to pulmonary pathology, Heart 1997; 77: p.138-146.
Banning AP, Lewis NP, Northridge DB, Elbom JS, Henderson AH, Perfusion/ventilation mismatch during exercise in chronic heart failure: an investigation of circulatory determinants. Br Heart J 1995; 74: p.27-33.
Buller NP, Poole-Wilson PA, Mechanism of the increased ventilatory response to exercise in patients with chronic heart failure. Heart 1990; 63; p.281-283.

