- Updated on October 29, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
Difficulty Breathing: Caused by Low Body O2
 Difficulty breathing (aka dyspnea or shortness of breath) is labored breathing accompanied by an unpleasant awareness of one’s own breathing. Difficulty in breathing is commonly present in people with progressive heart disease, cystic fibrosis, HIV-AIDS, cancer, COPD, asthma, emphysema, pregnancy and many other conditions. Common triggers for difficulty breathing are anxiety, exertion, sleep, and eating or meals.
Difficulty breathing (aka dyspnea or shortness of breath) is labored breathing accompanied by an unpleasant awareness of one’s own breathing. Difficulty in breathing is commonly present in people with progressive heart disease, cystic fibrosis, HIV-AIDS, cancer, COPD, asthma, emphysema, pregnancy and many other conditions. Common triggers for difficulty breathing are anxiety, exertion, sleep, and eating or meals.
What causes Difficulty Breathing?
Minute ventilation rates (chronic diseases)
| Condition | Minute ventilation |
Number of people |
All references or click below for abstracts |
| Normal breathing | 6 l/min | – | Medical textbooks |
| Healthy Subjects | 6-7 l/min | >400 | Results of 14 studies |
| COPD | 14 (+-2) l/min | 12 | Palange et al, 2001 |
| COPD | 12 (+-2) l/min | 10 | Sinderby et al, 2001 |
| COPD | 14 l/min | 3 | Stulbarg et al, 2001 |
| Cancer | 12 (+-2) l/min | 40 | Travers et al, 2008 |
| Heart disease | 15 (+-4) l/min | 22 | Dimopoulou et al, 2001 |
| Heart disease | 16 (+-2) l/min | 11 | Johnson et al, 2000 |
| Heart disease | 12 (+-3) l/min | 132 | Fanfulla et al, 1998 |
| Heart disease | 15 (+-4) l/min | 55 | Clark et al, 1997 |
| Heart disease | 13 (+-4) l/min | 15 | Banning et al, 1995 |
| Heart disease | 15 (+-4) l/min | 88 | Clark et al, 1995 |
| Heart disease | 14 (+-2) l/min | 30 | Buller et al, 1990 |
| Heart disease | 16 (+-6) l/min | 20 | Elborn et al, 1990 |
| Pulm hypertension | 12 (+-2) l/min | 11 | D’Alonzo et al, 1987 |
| Asthma | 13 (+-2) l/min | 16 | Chalupa et al, 2004 |
| Asthma | 15 l/min | 8 | Johnson et al, 1995 |
| Asthma | 14 (+-6) l/min | 39 | Bowler et al, 1998 |
| Asthma | 13 (+-4) l/min | 17 | Kassabian et al, 1982 |
| Asthma | 12 l/min | 101 | McFadden, Lyons, 1968 |
| Cystic fibrosis | 15 L/min | 15 | Fauroux et al, 2006 |
| Cystic fibrosis | 10 L/min | 11 | Browning et al, 1990 |
| Cystic fibrosis* | 10 L/min | 10 | Ward et al, 1999 |
| CF and diabetes* | 10 L/min | 7 | Ward et al, 1999 |
| Cystic fibrosis | 16 L/min | 7 | Dodd et al, 2006 |
| Cystic fibrosis | 18 L/min | 9 | McKone et al, 2005 |
| Cystic fibrosis* | 13 (+-2) l/min | 10 | Bell et al, 1996 |
| Cystic fibrosis | 11-14 l/min | 6 | Tepper et al, 1983 |
| Diabetes | 12-17 l/min | 26 | Bottini et al, 2003 |
| Diabetes | 15 (+-2) l/min | 45 | Tantucci et al, 2001 |
| Diabetes | 12 (+-2) l/min | 8 | Mancini et al, 1999 |
| Diabetes | 10-20 l/min | 28 | Tantucci et al, 1997 |
| Diabetes | 13 (+-2) l/min | 20 | Tantucci et al, 1996 |
| Sleep apnea | 15 (+-3) l/min | 20 | Radwan et al, 2001 |
| Liver cirrhosis | 11-18 l/min | 24 | Epstein et al, 1998 |
| Hyperthyroidism | 15 (+-1) l/min | 42 | Kahaly, 1998 |
The Homepage of this site has an extended Table that provides many more health conditions (such as heart disease, diabetes, etc.) with the same general observation: too heavy breathing at rest. The cause of difficulty breathing is hyperventilation or alveolar hypocapnia (lack of CO2 in the lungs).
The normal breathing pattern at rest is imperceptible, inaudible and unnoticeable to others. It is small in tidal volume (500 ml for a 70-kg man), slow (12 breaths/min), light (6 L/min for minute ventilation), strictly nasal and diaphragmatic. Hyperventilation leads to alveolar hypocapnia and disrupts normal oxygen delivery due to:
– 1) reduced arterial oxygenation caused by lung pathologies (COPD, emphysema, cystic fibrosis, lung cancer, and so forth) or
– 2) arterial hypocapnia, leading to vasoconstriction and a suppressed Bohr effect – both of which reduce oxygen delivery to the tissues.
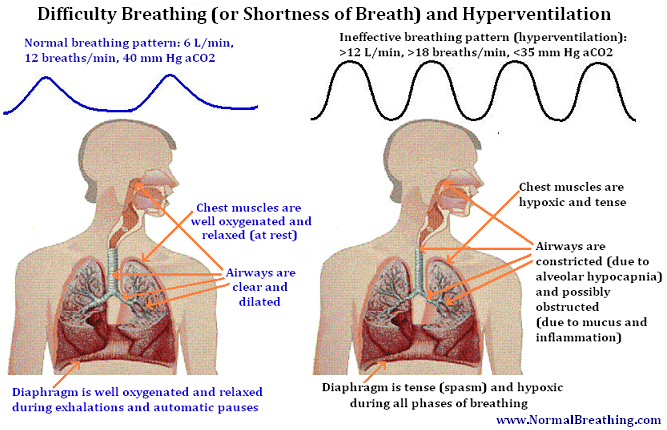
The factors that dramatically increase the work of breathing are constriction of airways due to alveolar hypocapnia, chest breathing (due to the spasmodic diaphragm), obstruction of airways due to mucus and chronic inflammation with possible a increase in blood viscosity.
Mouth breathing worsens difficulty breathing due to the reduction in NO (nitric oxide) absorption and reduced alveolar CO2.
Note that these people suffer from low O2 in cells and low CO2 in airways. CO2 in arterial blood can be high in those groups of people who develop problems with lungs. This will help to understand the title of this page.
Overeating (or eating meals), anxiety, stress, night sleep, deep breathing exercises, poor posture, and exertion all lead to more hyperventilation (and alveolar hypocapnia). As a result, it is obvious that they are triggers of breathing difficulties.
Treatment for Difficulty Breathing
Treatment of breathing difficulties should be based on a treatment of hyperventilation syndrome. Significant reduction in breathing difficulties has been achieved in tens of clinical trials after the application of various respiratory therapies and breathing devices. Patients need to achieve more than X seconds (see more below) for the body-oxygen test to prevent shortness of breath at rest.
When people have normal breathing (about 6 L/min with 10-12 breaths per minute and only 500-600 mL per breath), they generally do not feel their breathing, because normal breathing is tiny. Therefore, breathing normalization is the physiologically correct solution for this health problem with breathing difficulties.
As about the number X, it is provided right below here, as well as the best starting options (most effective treatment options) to get quick results in higher body oxygenation and fewer problems with difficulty breathing.
Get 20 s for the CP test to get rid of this symptom, and use breathing devices, such as the Frolov and DIY breathing devices to have quick easy progress.
[/sociallocker]

