- Updated on October 29, 2020
![]() By Dr. Artour Rakhimov, Alternative Health Educator and Author
By Dr. Artour Rakhimov, Alternative Health Educator and Author
- Medically Reviewed by Naziliya Rakhimova, MD
Severe Cancer: 25-40 Breaths/Min
Cancer Heavy Breathing and Dyspnea
This video is about Cancer Heavy Breathing and most effective known clinical trial on patients with metastatic cancer: Breathing and cancer.
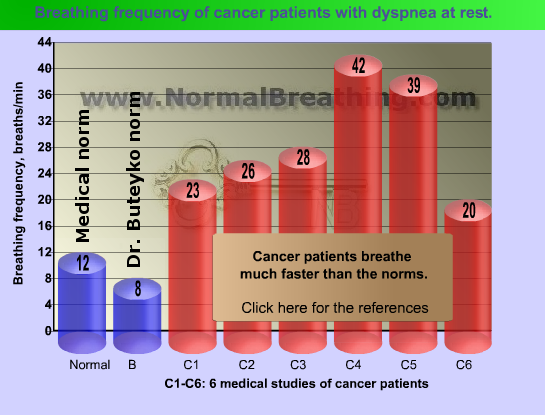
What is the typical breathing frequency in cancer patients with dyspnea? US medical doctors from the Massey Cancer Center (Virginia Commonwealth University in Richmond, Virginia, USA) tested 35 cancer patients (of the 35 patients, 34 were using oxygen) and found that their average breathing rate was 28.4 breaths/minute (Coyne et al, 2002). A 1993 study done by Italian and Canadian doctors revealed the respiratory rate of around 23 breathes per minute (Bruera et al, 1993) in a group of terminal cancer patients with dyspnea. A Swiss study conducted in the Division of Palliative Care, University Hospital, Lausanne found about 26 breaths per minute in elderly patients with advanced cancer (Mazzocato et al, 1999).
In two recent German studies (Department of Anaesthesiology, Intensive Care Medicine, Bonn), average breathing rates in 2 groups of cancer patients were stunning 42 and 39 breaths per minute (Clemens et al, 2007; Clemens et al, 2008). It is indeed physiologically shocking numbers since the normal respiratory frequency is only 12 breaths per one minute. (Old medical textbooks suggest 8-10 breaths per minute as normal.)
As we found before, the respiratory rate for the normal breathing pattern for adults is only 12 breaths/min at rest, while Dr. Buteyko’s norm is only 8 breaths per minute (see Parameters of Normal Breathing or Buteyko Table of Health Zones). here are respiratory rates in people with cancer.
We can see that cancer patients breathe much more than both norms. Furthermore, respiratory rate (breathing frequency) of cancer patients, as many studies have found, is an independent predictor of their mortality (Chiang et al, 2009; Groeger et al, 1998; de Miguel Sanchez et al, 2006). Those cancer sufferers, who breathe faster or more frequently, have higher mortality rates and poorer prognosis. This link (between slow spontaneous breathing and higher chances of survival) relates to all cancer patients, those with and without dyspnea.
Conclusion. Cancer patients: the faster they breathe, the sooner they die.
In 2008, the Journal of Applied Physiology published a study (Travers et al, 2008) from the Department of Medicine, Queen’s University (Kingston, Canada). It was revealed that forty patients with cancer breathed around 12 liters of air per minute at rest, instead of 6 l/min (the medical norm). The average breathing frequency of these cancer patients was 20 breaths per minute (the norm is only 12 breaths per min at rest). Tidal volume of these cancer patients (600 ml of air per one breath) was also more than the norm (which is 500 ml). Hence, these cancer patients had both, fast and deep breathing, in comparison with the medical norms.
We also learned that normal breathing is invisible and inaudible since it is very slow in frequency and tiny in tidal volume. What about visual breathing parameters of cancer patients at rest? In other words, what do the doctors see? Heavy breathing and nearly gasping for air.
After this overwhelming testimony of medical clinical doctors, it is more than clear that terminal cancer patients have heavy breathing patterns. (As we are going to learn later, that causes severe cell hypoxia that causes devastating effects on the immune system due to free radicals and oxidative damage.)
But normal breathing, as we discussed, (see Homepage links) is invisible, inaudible, and imperceptible. Moreover, according to physiological laws, normal breathing provides humans with superior tissue oxygenation. Hence, healthy people do not feel their breath at all. These cancer patients breathe at least 3-4 times more than the norm in order to be uncomfortably aware of their breathing.
References
Dyspnea references
Reuben DB, Mor V, Dyspnea in terminally ill cancer patients, Chest 1986; 89: p. 234–236.
Dudgeon DJ, Lertzman M, Dyspnea in the advanced cancer patient, J Pain Symptom Management 1998 Oct; 16(4): p.212–219.
Bruera E, MacEachern T, Ripamonti C, Hanson J, Subcutaneous morphine for dyspnea in cancer patients, Ann Intern Med. 1993; 119: p. 906–907.
Travers J, Dudgeon DJ, Amjadi K, McBride I, Dillon K, Laveneziana P, Ofir D, Webb KA, O’Donnell DE, Mechanisms of exertional dyspnea in patients with cancer, J Appl Physiol 2008 Jan; 104(1): p.57–66.
References for the cancer respiratory rate chart
Chiang JK, Lai NS, Wang MH, Chen SC, Kao YH, A proposed prognostic 7-day survival formula for patients with terminal cancer, BMC Public Health. 2009 Sep 29; 9(1): p.365.
Clemens KE, Klaschik E, Effect of hydromorphone on ventilation in palliative care patients with dyspnea, Support Care Cancer. 2008 Jan; 16(1): p.93–99. Epub 2007 Oct 11.
Clemens KE, Klaschik E, Symptomatic therapy of dyspnea with strong opioids and its effect on ventilation in palliative care patients, J Pain Symptom Management 2007 Apr; 33(4): p.473–481.
Coyne PJ, Viswanathan R, Smith TJ, Nebulized Fentanyl Citrate Improves Patients’ Perception of Breathing, Respiratory Rate, and Oxygen Saturation in Dyspnea, J Pain Symptom Manage 2002; 23: p.157–160.
de Miguel Sanchez C, Elustondo SG, Estirado A, Sanchez FV, de la Rasilla Cooper CG, Romero AL, Otero A, Olmos LG, Palliative Performance Status, Heart Rate and Respiratory Rate as Predictive Factors of Survival Time in Terminally Ill Cancer Patients, J Pain Symptom Managem. June 2006; 31(6), p. 485–492.
Groeger JS, Lemeshow S, Price K, Nierman DM, White P Jr, Klar J, Granovsky S, Horak D, Kish SK, Multicenter outcome study of cancer patients admitted to the intensive care unit: a probability of mortality model, J Clin Oncol. 1998 Feb; 16(2): p.761–770.
Mazzocato C, Buclin T, Rapin CH, The effects of morphine on dyspnea and ventilatory function in elderly patients with advanced cancer: a randomized double-blind controlled trial, Annals of Oncology. 1999 Dec; 10(12): p.1511–1514.